What is Cell Treatment?
Cell therapy is a treatment that uses living cells as drugs to treat disease asialogue. It takes
advantage of the immune system’s natural ability to recognise and destroy
abnormal cells in the body.
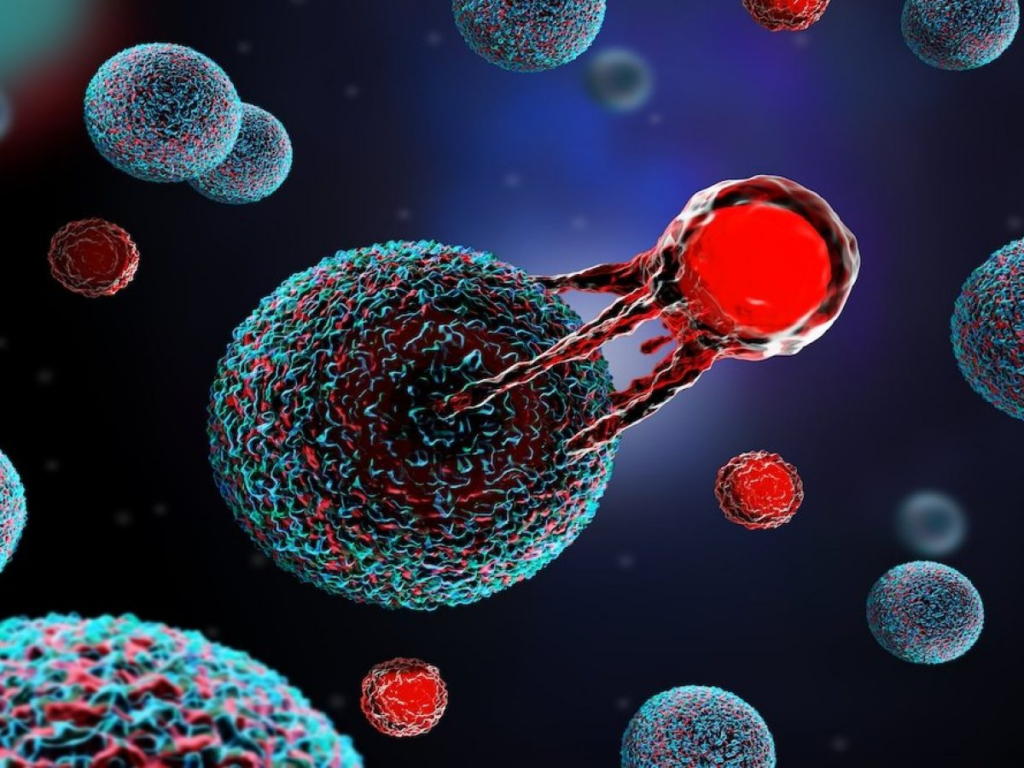
For example, in cancer cell therapy – also known as immune cell therapy or adoptive
cell therapy – specially engineered immune cells are targeted at tumours. These
cells can recognise cancer cells by their unique proteins or DNA that are processed
in a tumour and displayed on its surface. They can also target the cancer stem cells,
which are cells that give rise to tumours.
Scientists have been working for many years to develop cells that can be given to
patients to help fight their disease. There are now six approved cell therapies
available to treat people with some blood cancers and several more in early-stage
clinical trials.
Some types of cell therapy use stem cells, which are cells that can give rise to other
cells that can develop into specific tissues and organs. Others use other types of
cells, such as stromal cells (cells that support tissue growth and healing) and
mesenchymal stem cells (cells that can give rise to bone, cartilage and fat).
Stem cell therapy is one of the most exciting areas of medical research. It aims to
transform medicine by providing new approaches to treating and potentially curing
diseases that were once considered incurable.
There are two main types of stem cells – embryonic and adult. Embryonic stem cells
are taken from the human body’s early embryo and have properties similar to those
of all other cells in the body, including the ability to grow into any type of cell.
Scientists are using these cells to find ways of treating a wide range of conditions,
including neurodegenerative diseases and heart disease.
Adult cells are not taken from the human body’s embryo and have properties that
make them different to other cells in the body. They can be changed to have
properties of embryonic stem cells, which may allow scientists to produce a drug
that could treat a number of conditions. They can also be altered to stop the immune
system rejecting them.
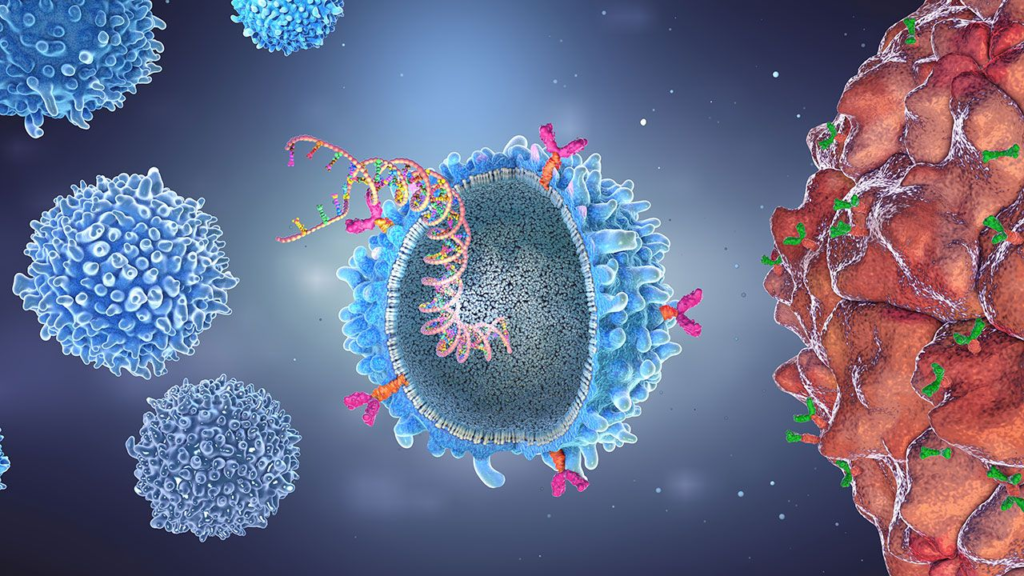
One example of this is chimeric antigen receptor T-cell (CAR T) therapy, which was
approved by the FDA for treating some B-cell cancers in 2017. It uses your own T
cells, which are removed from your blood and grown in the lab. They are then
‘customised’ in the lab by adding a gene to them that makes them recognise and
target a particular protein on your cancer cells. The modified T cells are then infused
back into your bloodstream.
The CAR T cells are able to attack and kill your cancer cells, which helps to improve
your chances of beating the disease. CAR T-cell therapies can reduce the need for
chemotherapy and other intensive treatments.
Your medical team will take a sample of your T cells from your blood in a process
called leukapheresis. They will then change them in the lab to add a genetically
engineered receptor called a CAR. The CAR T cells are then grown and infused back
into your bloodstream via a drip.
